
Professor Mikka Vikkula explains in his lecture how scientists are trying to identify the cause of vascular anomalies (including CMTC). The scientists search the DNA of patients for mutations that could be the cause of these disorders. So far, genes from 11 different hereditary vascular anomalies have been found. These genes have (a) mutation(s) as a result of which the gene -or actually the product, the protein- does not function properly. No specific gene of CMTC has been found yet.
Vikkula has been working in the field of vascular anomalies for over 20 years. After his training as a medical doctor he became very interested in human genetics during his postdoc period (1993-97) at Harvard Medical School, Boston, USA. He wanted to continue his work and started a new research group on human genetics at the De Duve Institute in Brussels in 1997. One of the subjects he he focuses on is vascular anomalies.
“About 20 years ago, all lesions were called an angioma or a hemoangioma. Today, we can distinguish 40 different types of vascular anomalies,” says Vikkula.
“A precise diagnosis is important to understand the development of the vascular anomaly, to be able to offer the best possible treatment and ultimately prevent the anomaly,” he stresses.
There are many different types of anomalies and many of them are in the skin, but they can also occur in any internal organ. Vascular anomalies can be hereditary or non-hereditary. Most are non-hereditary. In addition to increasing knowledge about these disorders, more and more specialized centers have been set up in the last years. These are multidisciplinary centers where doctors from different disciplines work together.
To be able to follow the rest of his story, he first explains something about DNA.
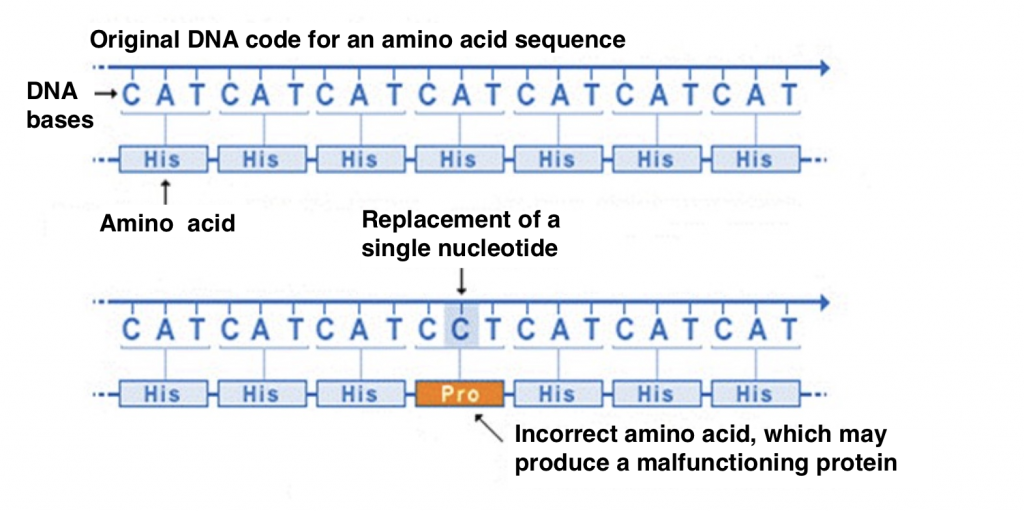
DNA consists of long strands of nucleotides containing different bases, A (adenine), C (cytosine), G (guanine) or T (thymine). These different nucleotide bases (abbreviated with the letters A, C, G and T) form the code with genetic instructions for the development, functioning, growth and reproduction of organisms. Each combination of three letters forms the code for a specific amino acid (for example: CAT = histidine, GTC and GTT = glutamine). Proteins consist of hundreds or thousands of amino acids, which are bound together in long chains. There are 20 different types of amino acids that can be combined to form a protein. There are many different types of proteins as the specific amino acid, the number and the sequence can vary. If one of the letters of the DNA is replaced by another letter (mutation), this can lead to a different amino acid and thus a different protein. Another protein can lead to a different function or no function at all which can cause a disease. A mutation in the DNA can also change the way an organ develops.
 How to detect mutations in DNA?
How to detect mutations in DNA?Every time a cell divides, it must make a complete copy of the DNA in the cell. This copying process is a source of errors. To find the errors we have to determine the sequence of the DNA (to read the DNA code). In order to determine the sequence of our DNA, it must first be cut into small fragments of 100 nucleotides. The sequencing machine can then determine the order of the nucleotides (letters) of the DNA. Then the fragments have to be put in the right order to reconstruct the whole DNA. In the sequencing work but also in the reconstitution work extra errors can occur, but there are ways to improve it and reduce the errors. We will not go into that further here.
Each individual has a slightly different DNA than another individual, which is why we are all different. Most differences in DNA are normal variations and do not cause disease. Very few variations can be the cause of disease. So how do you find variations (mutations) that cause vascular anomalies when 5000,0000 (5 million) variants can occur between two individuals? To simplify the work, you need to zoom in on the DNA that is most likely to contain the disease-causing mutation.
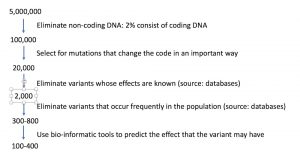
In the remaining DNA you have to look at the functions of the genes in which the variations occur. A gene is a piece of DNA that codes for a protein that has a function. In this research we are looking for genes that code for proteins that control vascular development. Are there already data about genes involved in vascular development? This way you can try to find the gene in question. Since 1994, genes from 11 different hereditary vascular abnormalities have been found. We can now test for these genetic abnormalities.
More information:
https://medlineplus.gov/genetics/understanding/mutationsanddisorders/genemutation/

Often a mutation causes the gene to lose its function or become less active, resulting in a disease/anomaly. TIE2 is an exception: certain mutations in this gene cause hyperactivation.
In 2009 we demonstrated for the first time that a non-hereditary vascular abnormality can be caused by single somatic mutations (i.e. mutations that are only present in the affected (malformed) areas). They are not transmitted from one generation to the next. Since then, not only the rare hereditary forms have been studied, but also the sporadic vascular abnormalities. The cause (somatic mutation) of Proteus syndrome was found in 2011 and CLOVES in 2013. Different diseases are now associated with different somatic mutations.
For example TIE2. This gene codes for a receptor on the outside of a cell membrane (see picture above). The mutation in TIE2 makes it too active. When activated, it will send too much signal into the cell. An inhibitor could slow down or inhibit the signal. Fortunately, different inhibitors have been developed for the different proteins that are being studied in the field of cancer. These proteins also play a role in vascular anomalies. We now use these inhibitors for vascular anomalies. Rapamycine/sirolimus is an inhibitor of mTOR (read more at: https://www.cmtc.nl/en/pedia/pedia-other/sirolimus/). It is now in phase 3 of a clinical study. This means that the final dosage will be tested for usability and effectiveness in larger numbers of patients. This will be compared with an existing drug or placebo. Safety in the short and long term is also investigated.
CMTC patients have red lesions at birth that (partly) fade away as they get older. Discoloration is much weaker. There is atrophy on the skin which distinguishes this condition from other anomalies. It is similar to capillary malformations. To find the gene for CMTC tissue is needed from the affected area and blood. Some capillary malformations have a PIK3CA mutation, some a GNAQ/GNA11 mutation. We do not see these mutations in CMTC. It could be a somatic mutation. If we find the gene or genes it gives us a diagnostic tool to identify CMTC and understand the underlying mechanism. Eventually we can develop a therapy.
Written by Dr. Lilian Vermeer





