
The rise of the laser in dermatology brought about a true revolution in the treatment of various skin conditions. Laser technologies have paved the way for both cosmetic and medical applications, providing dermatologists with a range of effective and safe treatment options. In this article we describe in a nutshell the history, contemporary applications and future of this special treatment modality.
Lasers in dermatology can be categorized by their wavelength and use (see Table 1). A distinction is made between ablative and non-ablative lasers. In short, the following applies: ablative lasers, such as the CO2 and Erbium-YAG lasers, remove thin layers of skin for resurfacing and wrinkle reduction, among other things. Fractionated lasers, including the fractionated CO2 and Erbium YAG lasers, create controlled microscopic damage for skin improvement. Non-ablative lasers, such as the Nd:YAG and diode lasers, heat deeper tissues without removing the skin. These are used for vascular lesions, skin tightening and hair removal, among other things. Pulsed dye lasers (PDL) emit laser light of a wavelength that is absorbed by hemoglobin, making them effective against vascular lesions, while the alexandrite and ruby lasers are suitable for pigmentation reduction and hair removal. The potassium titanyl phosphate (KTP) laser is used for vascular and pigmented lesions. Furthermore, some lasers are quality-switched (Q-switched), such as the Nd:YAG, ruby, alexandrite, and picosecond (pico) lasers, meaning they can generate very short, intense pulses of laser light. They are used for, among other things, tattoo removal, hair removal, pigment and skin improvement.
The word laser is an acronym of light amplification by stimulated emission of radiation. Every laser contains a laser medium, which is a material or gas mixture that can emit phased photons by light or electric current (stimulated emission). Lasers are regularly named after their laser medium. The introduction of lasers into dermatology occurred in the early 1960s. Maiman demonstrated the first functioning laser device, a ruby laser, in 1960, and in 1964 the Nobel Prize was awarded for fundamental research in quantum electronics, which provided the basis for the construction of today’s lasers. [2] Lasers were then quickly applied in various fields: telecommunications, aviation, space travel, photography, computer technology and medicine. The 1960s and 1970s saw many developments in the dermatological applications of laser devices, including the treatment of pigmented, (pre)malignant and vascular lesions. In 1984, the Food and Drug Administration (FDA) developed the first guidelines for the use of lasers for dermatological lesions. In the 1980s and 1990s, the first fractionated lasers were introduced, significantly improving the effectiveness of treatments and shortening recovery time for patients. In the 1990s, the applications of lasers were described for skin improvement, skin rejuvenation and hair removal, with Peter Velthuis increasing the applications of dermatological lasers in the Netherlands.
The carbon dioxide laser (CO2 laser) and the erbium-doped yttrium aluminum garnet laser (Erbium:YAG or Er:YAG laser) are two (fractionated) ablative lasers with a special place in contemporary practice. The CO2 laser uses carbon dioxide to generate laser energy, while the Er:YAG laser generates laser energy by using activated erbium ions in a crystalline medium.
The target chromophore for both is water; this results in photomechanical and photothermal effects in the skin, giving them an ablative effect. Thanks to the wavelength of the CO2 laser (10600 nm) and variability in duration of output (pulsed, continuous), the CO2 laser can achieve thermal effects in both the epidermis and deep dermis (Figure 1). The CO2 laser is therefore widely applicable for various medical indications, including rhinophyma, actinic keratosis/cheilitis, hypertrophic scars, keloid, epidermal nevi, neurofibromas and chondrodermatitis nodularis helicis. [1-2]
Figure 1. Schematic representation of the penetration depth into the skin of some ablative and non-ablative (fractional) lasers. [3]
The Er:YAG laser has a wavelength of 2940 nm and generally has a shorter pulse duration than the CO2 laser. With a shorter wavelength and higher absorption coefficient for water, the laser energy of the Er:YAG laser can achieve finer, more precise tissue ablation and the energetic penetration is lower, reaching the epidermis and (superficial) dermis (Figure 1). The Er:YAG laser therefore has a photomechanical effect (as opposed to a photothermal effect). [1] Because there are minimal thermal effects, there is also less collagen contraction than with the CO2 laser. Long-pulsed Er:YAG therefore generally achieves better clinical results than short-pulsed Er:YAG, and has fewer side effects than the CO2 laser. The Er:YAG laser can be used for acne scars, epidermal nevi, rhinophyma and neurofibromas, among others. [2]
In addition to the above medical indications, the CO2 and Er:YAG lasers are also used for skin tightening, wrinkle reduction and skin texture improvement. The Er:YAG laser works by controlled ablation of the epidermis. The laser energy is absorbed by the intra- and intercellular water, resulting in evaporation and removal of thin skin layers. This controlled removal stimulates collagen and elastin synthesis, leading to smoother skin texture, reduction of fine lines and improved firmness. The precision of the Er:YAG laser allows for precise control of the depth of treatment, making it suitable for superficial and deeper resurfacing.
The CO2 laser works through a similar ablation process. The fractionated CO2 laser emits the laser beams in the form of microscopic columns, creating controlled epidermal (and dermal) damage surrounded by healthy skin tissue (see Figure 1). This prevents excessive thermal necrosis, activates the skin’s intrinsic healing process and promotes collagen synthesis. It is suitable for photodamaged skin, wrinkles, dyschromias, atrophic scars and uneven skin texture. Due to the potentially longer recovery time and more pronounced results, it may be more suitable for patients with more obvious/severe skin problems.
Laser technology is continuously developing. For example, new lasers are being developed with unique properties that allow them to be used more accurately for specific conditions, but existing lasers are also being improved and, where possible, combined, making them even safer, more effective and more widely applicable.
There is an increasing shift towards non-invasive lasers that require minimal or no recovery time. This is mainly driven by the growing cosmetic applications of lasers. The request for cosmetic help is becoming increasingly common in the consultation room, partly due to the rise of social media and the concept of ‘flawless skin’ (perfect skin). The use of filters to smooth the skin in photos is becoming increasingly common. For this treatment requirement, lasers with a short downtime and collagen-stimulating properties are preferred.
Lasers may also be increasingly used for medical indications, whether or not in combination with other treatment modalities. Consider improved absorption of locally applied medications (laser-assisted drug delivery) or stem cell therapy in combination with laser therapy for wound healing, for example. [4-5] The usefulness of laser-assisted drug delivery is becoming increasingly clear and applied, especially in hypertrophic scars and keloids. Combination treatments increase effectiveness. Initially, vascular laser treatment is performed (for example using PDL/KTP/Nd:YAG), which reduces erythema and inflammation. The fractional CO2 laser is then used to create access to the dermis. Finally, a local medication is applied, for example a topical corticosteroid, such as clobetasol in ointment or triamcinolone acetonide intralesionally, but 5-fluorouracil in cream is also possible. [6] The treatment, or part of it, depending on what is still needed, is repeated several times (images 2, 3 and 4).
Finally, the dermatological indications of lasers will broaden, a recent example being the application of Er:YAG in Hailey-Hailey disease. [7] All in all, lasers will offer more and more treatment options, allowing treatments to be more personalized, in order to work more targeted with as little downtime and side effects as possible.
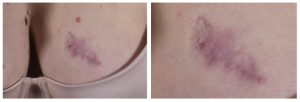
Figure 4. Scar after initial 3 KTP treatments and insufficient results good result after one-off combination of KTP, fractionated CO2 and clobetasol ointment.
The rise of the laser in dermatology has revolutionized the treatment of various skin conditions. Laser technologies have paved the way for both cosmetic and medical applications, providing dermatologists with a range of effective and safe treatment options. This article describes in a nutshell the history, contemporary applications and future of this special treatment modality. Laser technology continues to be developed, making it increasingly safer and effective, but also more personalized and can be used for more conditions.
Laser – dermatology – skin improvement – ablative and non-ablative – history – future
B. Razoki (Aios dermatologie, Maastricht UMC+),
T. Brinkhuizen (Dermatoloog, Maastricht UMC+ / Catharina Ziekenhuis Eindhoven)
Source: Nederlands tijdschrift voor Dermatologie & Venereologie, jaargang 33, nr.9, oktober 2023, blz.9-12





